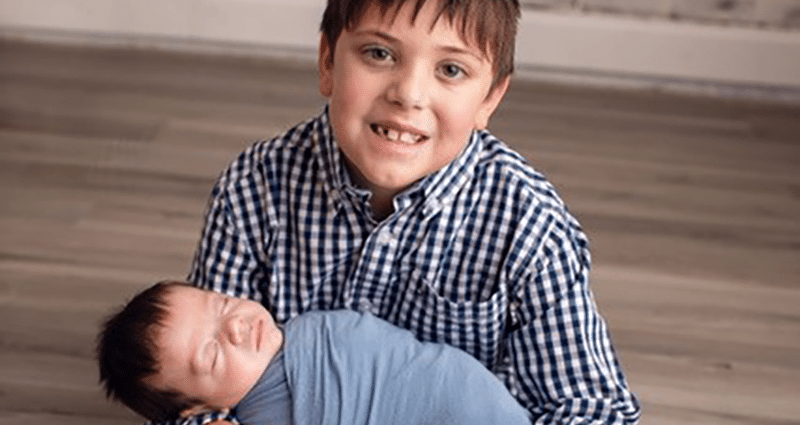
On a recent afternoon, Mia and Trent Boudreaux chatted about their family while their four-month-old son Ryland relaxed after a nap. Their older son, 8-year-old Tanner, was at school, where he is thriving after a summer growth spurt.
It might sound like an average day, but the Boudreauxes went through weeks where they didn’t know if their life would reach this point. Both of their sons regained their health after stays in the Neonatal Intensive Care Unit (NICU) at Our Lady of Lourdes Women’s & Children’s Hospital, where doctors and nurses went above and beyond to find solutions to the challenges that arose.
 “I definitely think the care they received got them to where they are today,” Mia said about her two young sons. “With Tanner, they tried everything possible to get his intubation tube in until it worked.
“I definitely think the care they received got them to where they are today,” Mia said about her two young sons. “With Tanner, they tried everything possible to get his intubation tube in until it worked.
When Ryland went through a cooling process, they were right by his side, making sure that he was as comfortable as possible. I’m not sure they would have gone from all of that to hitting every milestone now without Our Lady of Lourdes Women’s & Children’s.”
Mia’s pregnancy with Tanner took a turn at about 20 weeks, when doctors discovered she had an incompetent cervix. They inserted a stitch and put Mia on constant bed rest, but she was back at the hospital a little more than a week later because of hemorrhaging. Tanner was ultimately born at about 23 weeks.
“Tanner ended up being there 132 days,” Mia said. “From the very beginning, we saw how much they cared about him. One of his nurses, who has since become a good friend, sat for hours to get a central line in. They really became our family. We had every possible question and they answered all of them every single time.”
When the doctors finally determined Tanner was well enough to go home, the Boudreauxes were both excited and nervous. But, they were reassured by the fact that Our Lady of Lourdes Women’s & Children’s Hospital was just a few minutes away, meaning they wouldn’t have to travel far if Tanner needed additional care.
“We’ve had to make a couple of ER trips, and it’s always been important to us to get to a hospital quickly. Having a hospital like Our Lady of Lourdes Women’s & Children’s right here in Lafayette has made it easy,” Trent said. “I feel like we’re lucky to have it so close by.”
Because of the care they received with Tanner, the Boudreauxes knew they would go back to Our Lady of Lourdes Women’s & Children’s Hospital if they had another child. When Mia became pregnant with Ryland, they made arrangements for him to be born there. Things were progressing smoothly until Ryland suffered a lack of oxygen at birth, which can have long-term detrimental effects if not properly treated right away.
 “The nurse practitioner and nurse who were on call that night had also treated Tanner, so as scary as things were, it was nice to see the familiar faces in the NICU and know that Ryland would receive the same kind of quality care that Tanner had,” Mia said.
“The nurse practitioner and nurse who were on call that night had also treated Tanner, so as scary as things were, it was nice to see the familiar faces in the NICU and know that Ryland would receive the same kind of quality care that Tanner had,” Mia said.
Our Lady of Lourdes Women’s & Children’s Hospital, NICU Medical Director, Dr. Amy Zeringue, and neonatologist with Pediatrix Medical Group of Louisiana, said that care is rooted in a team approach that includes input from physicians, nurse practitioners, nurses, therapists, social workers, support staff and others. Whether the baby was born prematurely or needs extra help transitioning after being born at term, Dr. Zeringue said the staff takes cues from the babies and their families about the best course of action.
“The babies help us determine our plan of care every day,” she said. “We want to do enough to support them but also help them support themselves more so they can improve and we can take away some of those initial therapies.”
To ensure that babies in the NICU have the best chance at success, Dr. Zeringue said the physicians and staff continually stay up-to-date on the latest treatment methods. They regularly read new medical literature, attend conferences throughout the country to compare notes with other NICU practitioners and meet monthly with other groups to discuss new technology and case studies.
“Everything we do professionally is about being informed, learning about the different protocols and determining how we can improve outcomes,” she said. “The communication and collaboration with people across the country is really important and helpful for us.”
Ultimately, Ryland was in the NICU for nearly six weeks. During that time, the Boudreauxes remained impressed with both the medical care their son received as well as the way the staff took care of the whole family. A lactation nurse immediately recognized why Ryland was struggling with bottle feeding and helped solve the problem. Others answered questions, even if they came up more than once. And, Ryland’s grandparents were able to spend time with him in the NICU, giving them a chance to form early bonds.
“Trent and I couldn’t always be there because of work and the fact that I wasn’t driving,” Mia said. “It was a huge comfort to know that our parents could go and visit. I feel it’s important for our children to know the people who are going to surround them even when they’re newborns. The nurses and staff were great about it. It really felt like we were all helping each other out.”
 Dr. Zeringue said that building those relationships is key to successful outcomes, especially since multiple studies have shown that early interaction and touch helps babies thrive.
Dr. Zeringue said that building those relationships is key to successful outcomes, especially since multiple studies have shown that early interaction and touch helps babies thrive.
“One of the most important things is for our patients to experience love immediately, and there’s no greater love than from their families,” she said. “We incorporate a lot of that into our care, whether it’s holding the babies, talking to them in soothing voices or reading to them. All of that is a part of the neurological development we want our babies to have so they can continue to thrive in the world.”
Today, the Boudreauxes and many of the NICU staff have become close. They keep in contact via social media and phone calls. They celebrate birthdays and holidays together as a way to rejoice in how well the boys are doing as they both continue to grow.
 “Even though both of the experiences were scary, it was huge for us to have that hometown feeling,” Mia said. “You felt like it was family taking care of family, plus they have all of the latest technology and interventions to treat the babies. I talk to other moms on social media who have very different NICU experiences elsewhere, and I’m just so grateful that ours ended up being so positive.”
“Even though both of the experiences were scary, it was huge for us to have that hometown feeling,” Mia said. “You felt like it was family taking care of family, plus they have all of the latest technology and interventions to treat the babies. I talk to other moms on social media who have very different NICU experiences elsewhere, and I’m just so grateful that ours ended up being so positive.”
Dr. Zeringue said she and other staff members share in that joy and gratitude, especially as families like the Boudreauxes and others keep them updated about their children’s progress.
“It’s so rewarding and it reminds us on the really hard days to keep doing what we’re doing because it is making a difference,” she said. “I think we always feel really proud to see these kids go on to do great things. They always feel like part of our families and we’re still here to cheer them on and encourage them.”
Our Lady of Lourdes Women’s & Children’s Hospital provides the highest level of Neonatal Intensive Care in Acadiana. As the region’s only Level III Surgical NICU, we provide comprehensive care to infants born at all gestational ages and birth weights. For more information visit LourdesRMC.com/NICU.
We hope your family never needs a NICU, but it’s good to know what’s available — just in case. Across our health system we offer access to the highest quality family-centered care:
-
Greater Baton Rouge and Northshore: Our Lady of the Lake Children’s Hospital’s Newton & Betsy Thomas Family Center for Newborn & Infant Intensive Care
-
Acadiana: Our Lady of Lourdes Women’s & Children’s Hospital’s Level III Surgical NICU
-
Northeast Louisiana: the region’s only Level III NICU at St. Francis Medical Center