You might not know what sepsis is, but its impact is incredibly deadly. One in three patients who die in a hospital bed had sepsis during their hospitalization, and it’s the leading reason why a patient is admitted to the hospital or readmitted due to complications after their discharge.
It’s more deadly than breast cancer, prostate cancer and opioid overdoses, yet it’s also one of the most difficult diseases to diagnose.
For the past year, Franciscan Missionaries of Our Lady Health System has shown that those numbers can change. With a simple test that’s the first of its kind in any hospital, our care teams are saving lives. And this technology is expanding into our emergency rooms in several regions we serve.
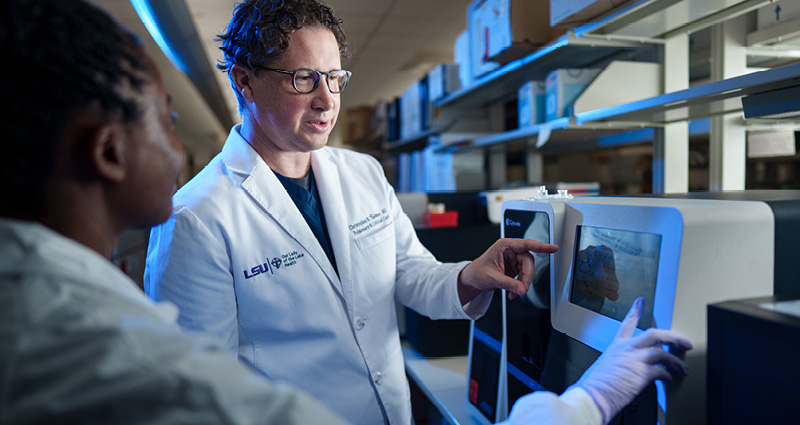
“This is the kind of situation where other healthcare systems are now looking to us as a model to follow,” says Christopher Thomas, MD, vice president and chief quality officer for Franciscan Missionaries of Our Lady Health System. “We’re setting the standard for emergency care and we’re more committed to taking care of sepsis than anyone else.”
Let’s take a look at how.
What is Sepsis?
Sepsis is the body’s extreme overreaction to infection. It could be due to an accident, organ failure, a ruptured appendix or any number of conditions where the body’s white blood cells would typically move into action, working hard to fight off infection. Except with sepsis, the white blood cells lose track of their mission and begin attacking indiscriminately – even attacking vital organs.
Symptoms for sepsis can sometimes be hard to differentiate from the symptoms of whatever condition brought you to the hospital in the first place – things like chills, fever, lightheadedness or confusion.
That’s why care teams in emergency rooms often misdiagnose sepsis, or delay treatment while they tackle your primary condition. If not treated early enough, sepsis can result in tissue damage, organ failure and death.
It’s the leading cause of death in hospitals and responsible for more than 270,000 deaths every year in the U.S., according to the Sepsis Alliance.
And whereas patients who come to the emergency room with a heart attack or stroke are treated using medically standardized tests (such as an EKG or CT scan), there’s been no universally agreed upon method to test for sepsis.
Until now.
What Our Research Found
Since 2014, Our Lady of the Lake Health in Baton Rouge and the LSU Health Sciences Center have partnered with medical diagnostics company Cytovale on more than half a dozen studies that led to a groundbreaking tool for emergency rooms.
It’s a test that uses a patient’s blood sample to examine white blood cells. The test literally “squishes” the cells to see how they react: Healthy cells will typically bounce back after being squished, while septic cells will stretch or flatten out as a result.
Based on these findings, Cytovale and Our Lady of the Lake collaborated to build a machine, known as IntelliSep, that can perform the test in under 10 minutes. The results of the test put patients in three possible categories:
- Not likely to be septic (therefore, their care can continue as normal)
- Possibly septic (more monitoring is needed)
- Likely to be septic (meaning action should be taken to treat them immediately)
This innovative tool has changed the game for sepsis treatment, helping Our Lady of the Lake’s emergency room teams identify patients who may be septic much faster, and getting them the right care quicker.
The IntelliSep test became operational in Our Lady of the Lake Regional Medical Center’s emergency department in August 2023.
Now, a year later, we’re already seeing incredible results and positive impacts on patients. We’re implementing this technology in nearly every region we serve in Louisiana and Mississippi.
And we’re also leading the way for other hospitals across the country to put this life-saving technology into action.
How We’re Saving Patients’ Lives
When you arrive at an emergency room with a life-threatening condition, minutes make all the difference.
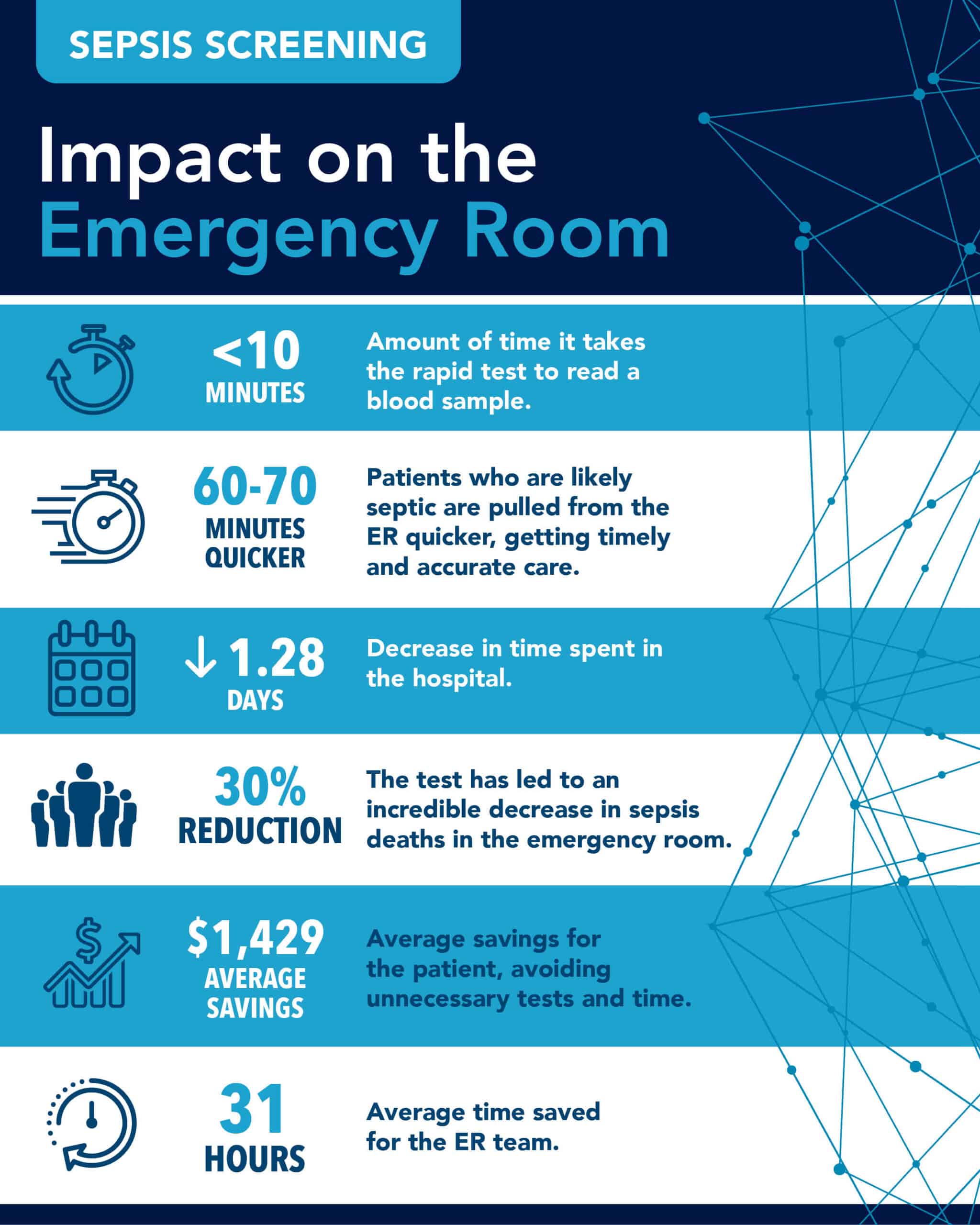
Since the IntelliSep test was installed at Our Lady of the Lake Regional Medical Center’s emergency room, any patient suspected of being septic has had a blood draw examined by the machine. If the results show the likelihood of sepsis, that patient is pulled from the waiting room 60 to 70 minutes earlier than they would have otherwise in order to begin treatment.
Getting care faster also speeds up recovery, meaning patients can leave the hospital faster than before. Length of stay averages have been reduced by 1.28 days for general inpatients and 2.24 days for ICU patients.
That reduction in length of stay means a lower cost of care for patients, too. Our Lady of the Lake’s findings since implementing IntelliSep show a cost of care reduction of $1,429 per patient.
It also reduced the amount of time our emergency room teams spend on unnecessary testing and other procedures to investigate a patient’s condition, saving about 31 hours of time.
These findings are incredible, but they are only the beginning as Our Lady of the Lake continues to formalize the test in our emergency department.
“It has put a spotlight on the incredible work our research teams have done and continue to do,” says Dr. Thomas. “And now that it’s operational in our emergency department and saving lives every day, it’s put a spotlight on how we’re implementing this technology, how we’ve established best practices, and how we’re truly leading the way.”